People with an acquired brain injury are protected under law by The UN Convention of Rights of Persons with Disabilities, an international agreement drawn up by countries who are members of the United Nations to support disabled people. The agreement takes a “rights based approach” by stating that people are:
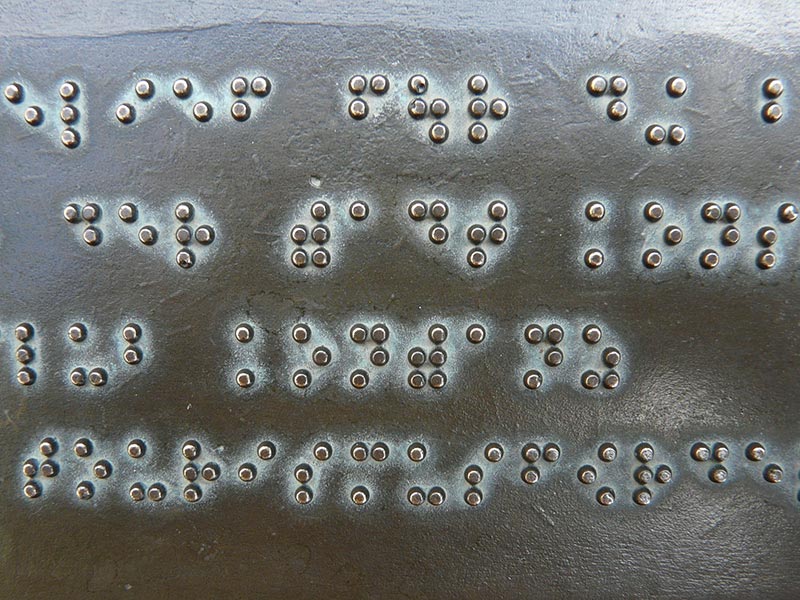
Essentially, this agreement gives disabled people the same rights as everybody else and seeks to protect them from prejudice and discrimination. This is achieved by giving disabled people equal access to services and opportunities through the making or changing of laws to protect their rights and making it illegal to break the laws within this agreement. Governments and authorities have the responsibility for ensuring that no discrimination takes place and that services are designed for everyone to access. This could be through the use of new technologies to help disabled people or by giving them accessible information to help them. Accessible information could include:
Countries that have signed up to this agreement promise to give disabled people equal access to housing, education and health care. It is agreed that disabled people have the same right to life and the same chances as everyone else. The UK, the Human Rights Act 1998 also protects disabled people.
The agreement makes special reference to social groups such as disabled women and children to make sure they are treated fairly and equally.
Countries make a pledge to raise awareness about the rights of disabled people by:
What rights should a disabled person be entitled to?
Mae pobl ag anaf i'r ymennydd yn cael eu diogelu o dan y gyfraith gan Gonfensiwn y Cenhedloedd Unedig ar Hawliau Pobl ag Anableddau, cytundeb rhyngwladol a luniwyd gan wledydd sy'n aelodau o'r Cenhedloedd Unedig i gefnogi pobl anabl. Mae'r cytundeb yn "ddull seiliedig ar hawliau" trwy ddatgan:
Yn ei hanfod, mae'r cytundeb hwn yn rhoi'r un hawliau i bobl anabl â phawb arall ac yn ceisio'u diogelu rhag rhagfarn a gwahaniaethu. Cyflawnir hyn drwy roi mynediad cyfartal i bobl anabl i wasanaethau a chyfleoedd drwy wneud neu newid cyfreithiau er mwyn diogelu eu hawliau a'i gwneud yn anghyfreithlon i dorri'r deddfau o fewn y cytundeb hwn. Mae llywodraethau ac awdurdodau yn gyfrifol am sicrhau nad oes gwahaniaethu yn digwydd a bod gwasanaethau'n cael eu cynllunio er mwyn i bawb allu eu defnyddio. Gallai hyn fod drwy ddefnyddio technolegau newydd i helpu pobl anabl neu drwy roi gwybodaeth hygyrch iddynt i'w helpu. Gallai gwybodaeth hygyrch gynnwys:
Mae gwledydd sydd wedi ymrwymo i'r cytundeb hwn yn addo rhoi mynediad cyfartal i dai, addysg a gofal iechyd i bobl anabl. Cytunir bod gan bobl anabl yr un hawl i fywyd a'r un cyfleoedd â phawb arall. Yn y DU, mae Deddf Hawliau Dynol 1998 hefyd yn diogelu pobl anabl.
Mae'r cytundeb yn cyfeirio'n arbennig at grwpiau cymdeithasol fel menywod a phlant anabl er mwyn sicrhau eu bod yn cael eu trin yn deg ac yn gyfartal.
Mae gwledydd yn gwneud adduned i godi ymwybyddiaeth am hawliau pobl anabl trwy:
Pa hawliau y dylai person anabl fod â hawl i'w cael?
The Medical Model of Disability
A definition of a medical model of disability is:
“Disabled people are seen as disabled due to their impairment (for example, blindness). If the impairment is cured, the issue of how a disabled person fits into society goes away and society doesn’t have to change to accommodate them.”www.allfie.org.uk (https://bit.ly/2LUme68)
The medical model of disability has negative effects for disabled people who are unable to be cured of their disability and means that they are unable to access the same education, work and social opportunities as others in society. This does not give them a rights-based approach to their disability and has far-reaching effects on their opportunities and quality of life. The medical model of disability focusses on what is “wrong” with a person instead of what their needs are. This creates low expectations and ultimately leads to loss of independence.
The Social Model of Disability
A definition of a social model of disability is:
“Disabled people are seen as being disabled not by their impairments (such as blindness or autism) but by society’s failure to take their needs into account. Being disabled is part of the normal spectrum of human life: society must expect disabled people to be there and include them.”www.allfie.org.uk (https://bit.ly/2YY1MVM)
The social model of disability states that disability is caused by the way that society is organised rather than a person’s impairment. The model investigates ways to remove barriers hence removing restrictions and allowing disabled people to live an independent and equal life.
This model allows disabled people to access a full range of educational, employment and social opportunities, giving them equal status and a better quality of life.
An example of how the social model of disability benefits disabled people in education is through adapting, not just the buildings of a school, but the curriculum and school ethos, allowing education to be inclusive and accessible for all.
Many disabled charities and organisations use the social model of disability as it was developed by disabled people and takes the view that people are disabled by barriers in society, not by their impairment or difference. Physical barriers can include steps, doorways or accessible toilets. Social barriers relate to peoples’ attitudes towards disabled people, for example, the assumption that they will not be able to carry out certain tasks.
Active Support model
This is a person-centred model based on interaction with individuals through a daily planning system that promotes participation and enhances quality of life. This model establishes the level of participation in activities and the level of support needed to develop the skills to engage in activities as independently as possible. Daily plans are based around positive interaction and reinforcement, teaching and relearning skills to participate in a range of valued and meaningful activities.
Questions
1. How would the social model of disability help a person with a brain injury who wants to access a building with steps and is struggling to walk again?
2. How would the social model of disability help a brain injury patient who has been left with language difficulties and wants to live independently in a rented property?
Y Model Meddygol o Anabledd
Dyma ddiffiniad o fodel meddygol o anabledd:
"Mae pobl anabl yn cael eu hystyried yn anabl oherwydd eu nam (er enghraifft, dallineb). Os caiff y nam ei wella, mae'r mater sy'n ymwneud â sut mae person anabl yn ffitio i mewn i gymdeithas yn mynd i ffwrdd ac nid oes yn rhaid i gymdeithas newid i ddarparu ar eu cyfer."Cyfieithiad o www.allfie.org.uk (https://bit.ly/2LUme68)
Mae'r model meddygol o anabledd yn arwain at effeithiau negyddol i bobl anabl nad oes modd eu gwella o'u hanabledd ac sy'n golygu nad ydynt yn gallu cael yr un cyfleoedd addysg, gwaith a chymdeithasol ag eraill mewn cymdeithas. Nid yw hyn yn rhoi dull gweithredu seiliedig ar hawliau iddynt o ran eu hanabledd ac mae'n cael effaith bellgyrhaeddol ar eu cyfleoedd ac ansawdd eu bywyd. Mae'r model meddygol o anabledd yn canolbwyntio ar yr hyn sy'n "anghywir" gydag unigolyn yn hytrach na beth yw ei anghenion. Mae hyn yn creu disgwyliadau isel ac yn arwain yn y pen draw at golli annibyniaeth.
Y Model Cymdeithasol o Anabledd
Dyma ddiffiniad o fodel cymdeithasol o anabledd:
"Mae pobl anabl yn cael eu hystyried yn anabl nid oherwydd eu namau (fel dallineb neu awtistiaeth) ond oherwydd methiant cymdeithas i ystyried eu hanghenion. Mae bod yn anabl yn rhan o sbectrwm arferol bywyd dynol: rhaid i Gymdeithas ddisgwyl i bobl anabl fod yno a'u cynnwys."Cyfieithiad o www.allfie.org.uk (https://bit.ly/2YY1MVM)
Mae'r model cymdeithasol o anabledd yn nodi bod anabledd yn cael ei achosi gan y ffordd y mae cymdeithas yn cael ei threfnu yn hytrach na nam unigolyn. Mae'r model yn ymchwilio i ffyrdd o gael gwared ar rwystrau, gan ddileu cyfyngiadau a chaniatáu i bobl anabl fyw bywyd annibynnol a chyfartal.
Mae'r model hwn yn galluogi pobl anabl i fanteisio ar ystod lawn o gyfleoedd addysgol, cyflogaeth a chymdeithasol, gan roi iddynt statws cyfartal ac ansawdd bywyd gwell.
Enghraifft o'r ffordd y mae'r model cymdeithasol o anabledd o fudd i bobl anabl mewn addysg yw drwy addasu, nid dim ond adeiladau ysgol, ond y cwricwlwm a'r ethos ysgol, gan ganiatáu i addysg fod yn gynhwysol ac yn hygyrch i bawb.
Mae llawer o elusennau a sefydliadau anabl yn defnyddio'r model cymdeithasol o anabledd gan iddo gael ei ddatblygu gan bobl anabl ac mae o'r farn mai rhwystrau yn y gymdeithas sy'n eu hanalluogi, nid nam neu wahaniaeth. Gall rhwystrau corfforol gynnwys grisiau, drysau neu doiledau hygyrch. Mae rhwystrau cymdeithasol yn ymwneud ag agweddau pobl tuag at bobl anabl, er enghraifft, y dybiaeth na fyddant yn gallu cyflawni rhai tasgau.
Model Cymorth Gweithredol
Model sy'n canolbwyntio ar yr unigolyn yw hwn sy'n seiliedig ar ryngweithio ag unigolion drwy system gynllunio ddyddiol sy'n hyrwyddo cyfranogiad ac yn gwella ansawdd bywyd. Mae'r model hwn yn sefydlu lefel y cyfranogiad mewn gweithgareddau a lefel y cymorth sydd ei angen i ddatblygu'r sgiliau i gymryd rhan mewn gweithgareddau mor annibynnol â phosibl. Mae cynlluniau dyddiol yn seiliedig ar ryngweithio ac atgyfnerthu cadarnhaol, sgiliau addysgu ac ailddysgu i gymryd rhan mewn amrywiaeth o weithgareddau gwerthfawr ac ystyrlon.
Cwestiynau
1. Sut fyddai'r model cymdeithasol o anabledd yn helpu rhywun sydd ag anaf i'w ymennydd sydd am gael mynediad i adeilad gyda grisiau ac sy'n cael trafferth cerdded eto?
2. Sut fyddai'r model cymdeithasol o anabledd yn helpu claf ag anaf i'r ymennydd ac sydd wedi'i adael gydag anawsterau iaith ac eisiau byw'n annibynnol mewn eiddo ar rent?

A hidden disability
Brain injury is often described as a hidden disability due to the lack of outward physical symptoms. A person with a brain injury may appear to be unaffected by illness and is therefore treated by others as an able-bodied person. Due to the lack of visible symptoms, other indications of brain injury such as depression, fatigue, altered appetite, memory and concentration problems are not always considered fully by carers of brain injury patients. For this reason, many reablement programmes try to involve family, friends and carers in rehabilitation to develop an understanding of the hidden symptoms. A brain injury patient may appear to have a changed personality due to anxiety, frustration, anger or problems listening or understanding. Family members sometimes feel that these changed behaviours are deliberate and fail to compensate for them. Some brain injury patients suffer from fatigue and find it difficult to regain their former conversational skills. Lack of compassion from their family can discourage them in their attempts to engage with others. Likewise, due to a lack of self-awareness following a brain injury, family members report that the patient lacks understanding of the difficulties in caring for them.
Many specialist brain injury hospitals offer support for families and carers as well as the patient in order to overcome the issues surrounding hidden symptoms.
The government have recognised hidden disabilities in their overhaul of the Blue Badge scheme. From 2019, people with hidden disabilities such as mental health and neurological conditions have access to the Blue Badge scheme which removes the barrier of travel for people who previously were unable to walk long distances or take public transport.
The Minister for Disabled People, Health and Work stated “We’re taking an important step forward in ensuring people with hidden disabilities get the support they need to live independently.”
Anabledd cudd
Mae anaf i'r ymennydd yn aml yn cael ei ddisgrifio fel anabledd cudd oherwydd diffyg symptomau corfforol allanol. Efallai y bydd person ag anaf i'r ymennydd yn ymddangos nad effeithir arno gan salwch ac felly caiff ei drin gan eraill fel person abl yn gorfforol. Oherwydd y diffyg symptomau gweladwy, nid yw arwyddion eraill o anaf i'r ymennydd megis iselder, blinder, chwant bwyd newidiedig, y cof a phroblemau canolbwyntio bob amser yn cael eu hystyried yn llawn gan ofalwyr cleifion sy'n dioddef anaf i'r ymennydd. Am y rheswm hwn, mae llawer o raglenni ail-alluogi yn ceisio cynnwys teulu, ffrindiau a gofalwyr mewn adsefydlu er mwyn datblygu dealltwriaeth o'r symptomau cudd. Mae'n bosibl y bydd newid ym mhersonoliaeth claf ag anaf i'r ymennydd oherwydd pryder, rhwystredigaeth, dicter neu broblemau wrth wrando neu ddeall. Mae aelodau'r teulu weithiau'n teimlo bod y newid hwn mewn ymddygiad yn fwriadol ac yn methu â gwneud iawn amdano. Mae rhai cleifion ag anaf i'r ymennydd yn dioddef blinder ac yn ei chael yn anodd adennill eu hen sgiliau sgwrsio. Gall diffyg tosturi gan eu teulu eu hannog i beidio â gwneud ymdrech i ymgysylltu ag eraill. Yn yr un modd, oherwydd diffyg hunanymwybyddiaeth yn dilyn anaf i'r ymennydd, mae aelodau o'r teulu yn dweud nad oes gan y claf ddealltwriaeth o'r anawsterau wrth ofalu amdanynt.
Mae llawer o ysbytai arbenigol ar gyfer anafiadau i'r ymennydd yn cynnig cymorth i deuluoedd a gofalwyr yn ogystal â'r claf er mwyn goresgyn y problemau sy'n gysylltiedig â symptomau cudd.
Mae'r llywodraeth wedi cydnabod anableddau cudd wrth ailwampio cynllun y Bathodyn Glas. O 2019, mae pobl sydd ag anableddau cudd megis cyflyrau iechyd meddwl a chyflyrau niwrolegol yn gallu manteisio ar gynllun y Bathodyn Glas sy'n cael gwared ar y rhwystr teithio i bobl nad oeddent yn gallu cerdded yn bell o'r blaen, na defnyddio trafnidiaeth gyhoeddus.
Dywedodd y Gweinidog dros Bobl Anabl, Iechyd a Gwaith "Rydym yn cymryd cam pwysig ymlaen o ran sicrhau bod pobl ag anableddau cudd yn cael y cymorth sydd ei angen arnynt i fyw'n annibynnol."
Health care professionals work under strict ethical codes of conduct stating that they must behave in an expected manner. Codes of conduct aim to protect service users and carers by ensuring that health professionals communicate effectively, manage risk and remain up to date with their knowledge and skills.
A rights-based approach is considered to be best practise by allowing health professionals to work within their ethical code of conduct. This approach sends a clear message to society that disabled people are on an equal footing with the rest of the population, having the same human rights. The social model of disability reinforces this thinking.
The rights-based approach improves the decision-making process for people with an acquired brain injury which, in turn, improves the quality and effectiveness of their health and social care.
This approach allows health and social care professionals to have a better understanding of the cultural and societal barriers that affect an individual’s health and well-being, enabling obstacles to be overcome and reablement to occur effectively.
All health and social care workers should be aware of the rights of individuals through the Human Rights Act 1998 and should know how to apply the contents of the Act in a practical way to disabled people. They should demonstrate their understanding that all disabled people have rights by communicating effectively and ensuring that information about services is accessible and can be understood.
A rights-based approach gives individuals the opportunity to be consulted in decisions and it should be assumed that they have the capacity to make decisions independently. If this is not the case, a person should have an advocate who is able to represent their views and opinions and can discuss their needs, concerns and priorities.
The Disability Discrimination Act
The Disability Discrimination Act gives disabled people the right to register with and access health and social care services such as GP surgeries, hospitals and dental surgeries. It also gives them the right to information in an accessible form which may be braille for those with visual impairments or an interpreter for those with hearing impairments. The DDA reinforces the rights-based approach by protecting individuals from discrimination.
Mae gweithwyr gofal iechyd proffesiynol yn gweithio o dan godau ymddygiad moesegol llym, gan ddatgan bod yn rhaid iddynt ymddwyn mewn modd disgwyliedig. Mae codau ymddygiad yn anelu at amddiffyn defnyddwyr gwasanaeth a gofalwyr drwy sicrhau bod gweithwyr iechyd proffesiynol yn cyfathrebu'n effeithiol, yn rheoli risg ac yn parhau i fod â'r wybodaeth a'r sgiliau diweddaraf.
Ystyrir bod dull gweithredu seiliedig ar hawliau yn arfer gorau drwy ganiatáu i weithwyr iechyd proffesiynol weithio o fewn eu cod ymddygiad moesegol. Mae'r dull hwn yn anfon neges glir i gymdeithas fod pobl anabl yn gydradd â gweddill y boblogaeth, ac yn meddu ar yr un hawliau dynol. Mae'r model cymdeithasol o anabledd yn atgyfnerthu'r meddylfryd hwn.
Mae'r dull gweithredu seiliedig ar hawliau yn gwella'r broses o wneud penderfyniadau i bobl ag anaf i'r ymennydd sydd, yn ei dro, yn gwella ansawdd ac effeithiolrwydd eu hiechyd a'u gofal cymdeithasol.
Mae'r dull hwn yn caniatáu i weithwyr proffesiynol ym maes iechyd a gofal cymdeithasol gael gwell dealltwriaeth o'r rhwystrau diwylliannol a chymdeithasol sy'n effeithio ar iechyd a llesiant unigolyn, gan alluogi goresgyn rhwystrau ac ail-alluogi i ddigwydd yn effeithiol.
Dylai pob gweithiwr iechyd a gofal cymdeithasol fod yn ymwybodol o hawliau unigolion drwy Ddeddf Hawliau Dynol 1998 a dylent wybod sut i gymhwyso cynnwys y Ddeddf mewn ffordd ymarferol i bobl anabl. Dylent ddangos eu bod yn deall bod gan bob unigolyn anabl hawliau drwy gyfathrebu'n effeithiol a sicrhau bod gwybodaeth am wasanaethau ar gael yn rhwydd ac y gellir ei deall.
Mae dull gweithredu seiliedig ar hawliau yn rhoi cyfle i unigolion ymgynghori mewn penderfyniadau a dylid cymryd yn ganiataol bod ganddynt y gallu i wneud penderfyniadau yn annibynnol. Os nad yw hyn yn wir, dylai fod gan berson eiriolwr sy'n gallu cyfleu ei farn a gall drafod ei anghenion, ei bryderon a'i flaenoriaethau.
Y Ddeddf Gwahaniaethu ar sail Anabledd
Mae'r Ddeddf Gwahaniaethu ar sail Anabledd yn rhoi'r hawl i bobl anabl gofrestru a chael gafael ar wasanaethau iechyd a gofal cymdeithasol megis meddygfeydd, ysbytai a deintyddfeydd. Mae hefyd yn rhoi hawl iddynt gael gwybodaeth ar ffurf hygyrch a allai gynnwys braille i rai â nam ar eu golwg neu gyfieithydd ar gyfer y rhai â nam ar eu clyw. Mae'r Ddeddf yn atgyfnerthu'r dull seiliedig ar hawliau drwy ddiogelu unigolion rhag gwahaniaethu.
Many people with an acquired brain injury report a feeling of worthlessness and despair. Able-bodied people often avoid individuals who are disabled and avoidance can exacerbate their situation. It is important that people living with an acquired brain injury feel inspired to recover their independence through living a valued and worthwhile life. A valued life is considered to be a lifestyle that has a balance of personal, social, vocational and educational elements to contribute to a good quality of life.
Each person has an individual view of what a valued life is, however, it is important to define standards and beliefs and to set personal goals to work towards. People recovering from a brain injury are encouraged to list the things that are important to them in order to set their own goals and targets. Many people do this through volunteering which gives them a sense of purpose and mental stimulation. Volunteering allows recovering patients the opportunity to help others without the commitment of full-time employment. It enables them to re-connect with people socially and re-develop language skills. This, in turn, reduces feelings of anxiety, anger and stress that are often associated with brain injury. The positive effects of volunteering combat depression and lead to the feeling of living a valued life through helping others. Volunteering gives individuals the sense of purpose and direction necessary for reablement and recovery.
Being valued means feeling appreciated by others and not belittled. This is an essential element of overcoming the barriers of being disabled and contributes to positive emotional, social and spiritual well-being. A full and valued life should include some or all of the following:
Taking a person-centred approach to engage an individual in meaningful activities is a beneficial way of helping them lead a valued life and therefore make a good recovery. Individuals should be supported to enable them to express their opinion, which may be difficult if speech and language functions have been impaired. Consideration and tolerance should be given to brain injury patients who have information processing issues or aphasia (loss of language skills). A person-centred approach allows individuals to identify what matters to them and set themselves personal goals which can be broken down into smaller, achievable steps. Goals should be measurable so that achieving gives a sense of accomplishment. A brain injury patient should decide who they would like to be involved in their reablement, how to involve key people where and when the person-centred planning should take place.
Mae llawer o bobl ag anaf i'r ymennydd yn dweud eu bod yn teimlo'n ddiwerth ac yn anobeithio. Bydd pobl sy'n abl yn gorfforol yn aml yn osgoi unigolion anabl ac mae osgoi'r unigolion hynny yn gwaethygu eu sefyllfa. Mae'n bwysig bod pobl sy'n byw gydag anaf i'r ymennydd yn teimlo eu bod yn cael eu hysbrydoli i wella eu hannibyniaeth drwy fyw bywyd gwerthfawr a gwerth chweil. Ystyrir bywyd gwerthfawr yn ffordd o fyw sydd â chydbwysedd o elfennau personol, cymdeithasol, galwedigaethol ac addysgol i gyfrannu at ansawdd bywyd da.
Mae gan bob unigolyn farn unigol ynglŷn â beth yw bywyd gwerthfawr, ond mae'n bwysig diffinio safonau a chredoau a gosod nodau personol i weithio tuag atynt. Mae pobl sy'n gwella o anaf i'r ymennydd yn cael eu hannog i restru'r pethau sy'n bwysig iddyn nhw er mwyn gosod eu nodau a'u targedau eu hunain. Mae llawer o bobl yn gwneud hyn drwy wirfoddoli sy'n rhoi ymdeimlad o bwrpas iddynt ac ysgogiad meddyliol. Mae gwirfoddoli yn caniatáu i gleifion sy'n adfer gael y cyfle i helpu eraill heb ymrwymiad cyflogaeth lawn-amser. Mae'n eu galluogi i ailgysylltu â phobl yn gymdeithasol ac i ail-ddatblygu sgiliau iaith. Mae hyn, yn ei dro, yn lleihau teimladau o bryder, dicter a straen sy'n aml yn gysylltiedig ag anaf i'r ymennydd. Mae effeithiau cadarnhaol gwirfoddoli yn gwrthsefyll iselder ac yn arwain at y teimlad o fyw bywyd gwerthfawr drwy helpu eraill. Mae gwirfoddoli yn rhoi i unigolion yr ymdeimlad o bwrpas a chyfeiriad sydd ei angen ar gyfer ail-alluogi ac adfer.
Mae cael eu gwerthfawrogi yn golygu teimlo bod pobl eraill yn eu gwerthfawrogi ac nad ydynt yn cael eu bychanu. Mae hyn yn elfen hanfodol o oresgyn y rhwystrau o fod yn anabl ac yn cyfrannu at lesiant emosiynol, cymdeithasol ac ysbrydol cadarnhaol. Dylai bywyd llawn a gwerthfawr gynnwys rhai neu bob un o'r canlynol:
Mae mabwysiadu ymagwedd sy'n canolbwyntio ar yr unigolyn er mwyn ymgysylltu ag unigolyn mewn gweithgareddau ystyrlon yn ffordd fuddiol o'u helpu i fyw bywyd gwerthfawr ac felly gwella'n dda. Dylai unigolion gael eu cefnogi i'w galluogi i fynegi eu barn, a all fod yn anodd os yw’r swyddogaethau lleferydd ac iaith wedi cael eu amharu. Dylid rhoi ystyriaeth a goddefgarwch i gleifion sydd ag anaf i'r ymennydd sydd â phroblemau prosesu gwybodaeth neu affasia (colli sgiliau iaith). Mae dull gweithredu sy'n canolbwyntio ar yr unigolyn yn caniatáu i unigolion nodi'r hyn sy'n bwysig iddynt a phennu nodau personol iddynt eu hunain y gellir eu rhannu'n gamau llai, cyraeddadwy. Dylai nodau fod yn fesuradwy fel bod cyflawni yn rhoi ymdeimlad o gyflawniad. Dylai claf ag anaf i’r ymennydd benderfynu pwy yr hoffai iddo fod yn rhan o'i ail-alluogi, sut i gynnwys pobl allweddol lle a phryd y dylai'r cynllunio sy'n canolbwyntio ar yr unigolyn ddigwydd.

The difficulties that a brain injury patient deals with during recovery are as follows:
Impairments of judgement and insight make managing risk particularly difficult and hard to manage without putting the patient in danger. A balance should be struck between encouraging independence and assessing the risk to avoid harm. A risk assessment should be carried out for activities that could be hazardous for brain injury patients and this is sometimes referred to as positive risk taking.
The brain is divided in two and connected by the corpus callosum.
The left hemisphere deals with logical thought processes, language, planning and analyzing.
The right hemisphere deals with social awareness, intuition and creativity.
In women the hemispheres are very well connected hence they can feel and think simultaneously but men have feeble connections so they can either listen OR use logic but not both together. For this reason, young males have the highest probability for exposure to risks and hazards.
The dorsolateral part of the brain deals with planning and prioritizing. Damage to this part of the brain can lead to a lack of contingency planning, thus increasing risk.
The mediofrontal part of the brain initiates activity. Damage to this part of the brain can lead to a lack of initiative and the inability to perform purposeful tasks.
The orbitofrontal part of the brain inhibits unwanted impulses and can lead to uninhibited and aggressive behavior which, again, increases risk.
Further complications in assessing and managing risk arise from the extreme fatigue that brain injury patients suffer from. This, together with prescribed medication, can result in hazards whilst driving, operating machinery and in social situations.
Positive risk taking and risk assessment
Weighing up the potential benefit and harm of one action over another can be difficult for patients with a brain injury. A positive risk management programme can be put in place through agreement with the individual, carers and health professionals which assesses the approaches needed to support identified risks.
Prior to discharge from hospital, a brain injury patient will undergo an assessment by a neuropsychiatrist who has expertise in managing individuals with emotional and behavioural difficulties following brain injury. A neuropsychiatrist considers emotions, perceptions, thought and cognitive processes in order to devise a plan in which risks can be managed safely.
Advice for health professionals and carers managing risk in conjunction with a brain injury patient is to be explicit about what the risks are, a risk assessment should be carried out and, should the patient not engage with this assessment, they should be discharged.
Negative risk and learned helplessness
The opposing behaviour to positive risk taking is the avoidance of risky or negative circumstances due to previous experience telling an individual that they may not have control over the situation. This is known as learned helplessness and results in a negative cycle of low expectations that are self-fulfilling creating a feeling of dependency on others, low self-esteem and a lack of self-belief.
Risk and social inclusion
The way in which a person responds to risk is partly down to social factors and partly biological factors and relates to their vulnerability and resilience. Reduced ability to communicate with and adapt in society increases the possibility a brain injury patient putting themselves at risk of danger and excluding themselves from society as a result.
Voice, choice and control
Giving people a voice, choice and control over decisions gives them a person-centred approach documented and applied by health professionals such as nurses, carers and support staff. It allows patients to have a voice and make their views known and to have maximum influence over decisions that affect their lives.
This approach states that:
The 2014 Social Services and Well-being (Wales) Act highlights the importance of balancing the risks of undertaking an activity with the risks to a person’s well-being in not being able to undertake that activity.
Taking an informed risk
An example of taking an informed risk after brain injury is driving. There are a number of skills such as physical movement of legs and arms and cognitive skills such as decision making and concentration which have to be coordinated whilst driving. Although many brain injury patients retain their former driving skills, taking an informed risk would entail undergoing a driving assessment before attempting to drive. This is, not only to establish if adaptations need to be made to the car, but to assess the risk of thinking, memory, judgement, decision-making and emotions on driving ability. If the risk is deemed to be low, a brain injury can regain a good level of independence through driving.
Dyma'r anawsterau y mae claf ag anaf i'r ymennydd yn delio â nhw yn ystod adferiad:
Mae amhariadau ar farn a mewnwelediad yn gwneud rheoli risg yn arbennig o anodd ac anodd ei reoli heb roi'r claf mewn perygl. Dylid sicrhau cydbwysedd rhwng annog annibyniaeth ac asesu'r risg er mwyn osgoi anaf. Dylid cynnal asesiad risg ar gyfer gweithgareddau a allai fod yn beryglus i gleifion ag anaf i'r ymennydd a chyfeirir at hyn weithiau fel cymryd risgiau cadarnhaol.
Mae'r ymennydd wedi'i rannu'n ddwy ac wedi'i gysylltu â'r corpus callosum.
Mae'r hemisffer chwith yn ymdrin â phrosesau meddwl rhesymegol, iaith, cynllunio a dadansoddi.
Mae'r hemisffer dde yn ymdrin ag ymwybyddiaeth gymdeithasol, greddf a chreadigrwydd.
Mewn merched mae'r hemisfferau wedi'u cysylltu'n dda iawn ac felly gallant deimlo a meddwl ar yr un pryd ond mae gan ddynion gysylltiadau gwan fel y gallant naill ai wrando NEU defnyddio rhesymeg ond nid y ddau gyda'i gilydd. Am y rheswm hwn, dynion ifanc sydd â'r tebygolrwydd mwyaf o ddod i gysylltiad â risgiau a pheryglon.
Mae rhan cefnystlysol yr ymennydd yn ymdrin â chynllunio a blaenoriaethu. Gall anaf i'r rhan hon o'r ymennydd arwain at ddiffyg cynllunio wrth gefn, a thrwy hynny gynyddu risg.
Mae'r rhan mediodalcennol o'r ymennydd yn cychwyn gweithgaredd. Gall anaf i'r rhan hon o'r ymennydd arwain at ddiffyg Menter a'r anallu i gyflawni tasgau pwrpasol.
Mae'r rhan craudalcennol o'r ymennydd yn llesteirio ysgogiadau diangen a gall arwain at ymddygiad anymatal ac ymosodol sydd, unwaith eto, yn cynyddu risg.
Mae cymhlethdodau pellach wrth asesu a rheoli risg yn deillio o'r blinder eithafol y mae cleifion ag anaf i'r ymennydd yn ei ddioddef. Gall hyn, ynghyd â meddyginiaeth ar bresgripsiwn, arwain at beryglon wrth yrru, gweithredu peiriannau ac mewn sefyllfaoedd cymdeithasol.
Cymryd risgiau cadarnhaol ac asesu risg
Gall pwyso a mesur y budd a'r anaf posibl i un weithred yn lle un arall fod yn anodd i gleifion sydd ag anaf i'r ymennydd. Gellir rhoi rhaglen rheoli risg gadarnhaol ar waith trwy gytundeb gyda'r unigolyn, gofalwyr a gweithwyr iechyd proffesiynol sy'n asesu'r dulliau sydd eu hangen i gefnogi risgiau a nodwyd.
Cyn eu rhyddhau o'r ysbyty, bydd claf ag anaf i'r ymennydd yn cael asesiad gan niwroseiciatrydd sydd ag arbenigedd mewn rheoli unigolion ag anawsterau emosiynol ac ymddygiadol yn dilyn anaf i'r ymennydd. Mae niwroseiciatrydd yn ystyried emosiynau, canfyddiadau, prosesau meddwl a gwybyddol er mwyn dyfeisio cynllun lle gellir rheoli risgiau yn ddiogel.
Cyngor i weithwyr iechyd proffesiynol a gofalwyr sy'n rheoli risg ar y cyd â chlaf ag anaf i'r ymennydd yw bod yn glir ynghylch beth yw'r risgiau, dylid cynnal asesiad risg ac, os na fydd y claf yn cymryd rhan yn yr asesiad hwn, dylid ei ryddhau.
Risg negyddol a diymadferthedd wedi'i ddysgu
Yr ymddygiad gwrthwynebol o ran cymryd risgiau cadarnhaol yw osgoi amgylchiadau peryglus neu negyddol oherwydd profiad blaenorol sy’n dweud wrth unigolyn nad oes ganddo reolaeth dros y sefyllfa o bosibl. Gelwir hyn yn ddiymadferthedd wedi'i ddysgu ac mae'n arwain at gylch negyddol o ddisgwyliadau isel sy'n hunangyflawnol gan greu teimlad o ddibyniaeth ar eraill, hunan-barch isel a diffyg hunangred.
Risg a chynhwysiant cymdeithasol
Mae'r ffordd y mae person yn ymateb i risg yn rhannol oherwydd ffactorau cymdeithasol a rhannol oherwydd ffactorau biolegol ac mae'n ymwneud â'u bregusrwydd a'u gwydnwch. Mae llai o allu i gyfathrebu â chymdeithas ac addasu iddi yn cynyddu'r posibilrwydd y bydd claf ag anaf i'r ymennydd yn peryglu ei hun ac yn cau ei hun allan o'r gymdeithas o ganlyniad.
Llais, dewis a rheolaeth
Mae rhoi llais, dewis a rheolaeth i bobl ar benderfyniadau yn rhoi dull sy'n canolbwyntio ar yr unigolyn iddynt sy’n cael ei gofnodi a'i gymhwyso gan weithwyr iechyd proffesiynol megis nyrsys, gofalwyr a staff cymorth. Mae'n galluogi cleifion i gael llais a lleisio'u barn a chael y dylanwad mwyaf posibl dros benderfyniadau sy'n effeithio ar eu bywydau.
Mae'r dull hwn yn nodi:
Mae Deddf Gwasanaethau Cymdeithasol a Llesiant (Cymru) 2014 yn pwysleisio pwysigrwydd cydbwyso’r risg o wneud gweithgaredd â’r risg i lesiant person os nad ydynt yn medru gwneud y gweithgaredd hwnnw.
Cymryd risg wybodus
Un enghraifft o gymryd risg wybodus ar ôl anaf i'r ymennydd yw gyrru. Mae nifer o sgiliau megis symudiadau corfforol coesau a breichiau a sgiliau gwybyddol megis gwneud penderfyniadau a chanolbwyntio y mae'n rhaid eu cydlynu wrth yrru. Er bod llawer o gleifion ag anaf i'r ymennydd yn cadw eu sgiliau gyrru blaenorol, byddai cymryd risg wybodus yn golygu cael asesiad gyrru cyn ceisio gyrru. Mae hyn, nid yn unig i sefydlu a oes angen gwneud addasiadau i'r car, ond i asesu'r risg o feddwl, cof, barnu, gwneud penderfyniadau ac emosiynau ar y gallu i yrru. Os bernir bod y risg yn isel, gall anaf i'r ymennydd adennill lefel dda o annibyniaeth drwy yrru.
Advocacy allows disabled people and vulnerable members of society to have their voice heard on issues that are important to them. An advocate defends and safeguards their rights by expressing views and concerns on their behalf. An advocate also accesses information and services and explores choices and options in order to promote their rights and responsibilities.
The advocacy service ensures that information is fully understood by a person, their rights have been clearly explained and that plans for their care say what they want.
This can include speaking in multi-agency meetings or writing letters.
Who can advocates be?
An advocate is bound by an ethical code of conduct in the same way as all professionals. The Advocacy Charter of July 2002 was set out with the “voice, choice, control” ethos and is a set of guidelines within which advocates work to represent a person’s interests, promoting social inclusion, equality and social injustice. An advocate can be a friend or family member (informal advocate) who is happy to speak on behalf of a person or could be an independent or formal advocate who is appointed and has received training in advocacy. Support from a person suffering from a similar disability is known as a peer advocate and is usually a volunteer. A citizen advocate works one to one with an individual and is independent of services and family, usually being a member of the local community. Collective advocacy occurs when a group of people facing a similar problem work together on a specific problem. When an individual with a disability such as brain injury is able to speak for themselves and represent their own views, this is known as self-advocacy. Self-advocacy groups are often set up to support self-advocates and build their confidence.
A non-instructed advocate
When a person lacks the mental capacity to appoint an advocate, but is able to express preferences such as a wish to return home from hospital, a non-instructed advocate may act on their behalf to make sure treatment is fair and decisions are taken with due consideration of all factors including a person’s individual preferences.
Advocates should be non-judgemental and impartial and should represent the wishes of the person they are representing. They should not compromise the independence of the person they are working on behalf of and should not undermine their confidence. This is known as a person-centred approach.
Advocacy should be provided free to people who are eligible for the service. Under the Care Act 2014, local authorities have a duty of care to offer an advocate during the assessment, planning, care review or safeguarding review stages of a person’s care providing they:
Substantial difficulty is deemed to be difficulty:
An appropriate adult cannot be:
Training for advocates
Independent advocates should adhere to the statutory guidance of the Regulation and Inspection of Social Care (Wales) Act 2016 (https://bit.ly/2PjvTFc) and work towards the National Qualification in Advocacy within one year of being appointed. This is a competency-based qualification for which evidence of real working practice must be submitted. Due to the close connection with the Mental Capacity Act, advocates may also study training units about “providing independent mental capacity advocacy” and “deprivation of liberty safeguards”.
Mae eiriolaeth yn caniatáu i bobl anabl ac aelodau bregus o gymdeithas leisio eu barn ar faterion sy'n bwysig iddynt. Mae eiriolwr yn amddiffyn ac yn diogelu eu hawliau drwy fynegi barn a phryderon ar eu rhan. Mae eiriolwr hefyd yn cyrchu gwybodaeth a gwasanaethau ac yn archwilio dewisiadau ac opsiynau er mwyn hybu eu hawliau a'u cyfrifoldebau.
Mae'r gwasanaeth eiriolaeth yn sicrhau bod unigolyn yn deall gwybodaeth yn llawn, bod eu hawliau wedi cael eu hegluro'n glir a bod cynlluniau ar gyfer eu gofal yn dweud yr hyn y maen nhw ei eisiau.
Gall hyn gynnwys siarad mewn cyfarfodydd aml-asiantaeth neu ysgrifennu llythyrau.
Pwy all eiriolwyr fod?
Mae eiriolwr yn rhwym wrth god ymddygiad moesegol yn yr un modd â phob gweithiwr proffesiynol. Cafodd Siarter Eiriolaeth Gorffennaf 2002 ei nodi gyda'r ethos "llais, dewis, rheolaeth" ac mae'n set o ganllawiau y mae eiriolwyr yn gweithio o'u mewn i gynrychioli diddordebau unigolyn, hyrwyddo cynhwysiant cymdeithasol, cydraddoldeb ac anghyfiawnder cymdeithasol. Gall eiriolwr fod yn ffrind neu'n aelod o'r teulu (eiriolwr anffurfiol) sy'n fodlon siarad ar ran person neu a allai fod yn eiriolwr annibynnol neu ffurfiol a benodir ac sydd wedi derbyn hyfforddiant mewn eiriolaeth. Mae cymorth gan berson sy'n dioddef o anabledd tebyg yn cael ei alw yn eiriolwr gan gymheiriaid ac mae fel arfer yn wirfoddolwr. Mae eiriolwr dinasyddion yn gweithio un i un gydag unigolyn ac yn annibynnol o wasanaethau a theulu, gan amlaf fel aelod o'r gymuned leol. Mae eiriolaeth ar y cyd yn digwydd pan fydd grŵp o bobl sy'n wynebu problem debyg yn gweithio gyda'i gilydd ar broblem benodol. Pan fydd unigolyn sydd ag anabledd, fel anaf i'r ymennydd, yn gallu siarad drosto'i hun a dangos ei farn ei hun, yr enw ar hyn yw hunan-eiriolaeth. Mae grwpiau hunan-eiriolaeth yn aml yn cael eu sefydlu i gefnogi hunan-eiriolwyr ac i adeiladu eu hyder.
Eiriolwr heb gyfarwyddyd
Pan nad oes gan berson y galluedd meddyliol i benodi eiriolwr, ond ei fod yn gallu mynegi ei ddymuniadau fel dymuniad i ddychwelyd adref o'r ysbyty, gall eiriolwr heb gyfarwyddyd weithredu ar ei ran i sicrhau bod triniaeth yn deg a bod penderfyniadau'n cael eu cymryd gydag ystyriaeth briodol o'r holl ffactorau gan gynnwys dewisiadau unigol unigolyn.
Dylai eiriolwyr fod yn anfeirniadol ac yn ddiduedd a dylent gynrychioli dymuniadau'r person y maent yn ei gynrychioli. Ni ddylent beryglu annibyniaeth y person y maent yn gweithio ar ei ran, ac ni ddylent danseilio eu hyder. Gelwir hyn yn ddull person ganolog.
Dylid darparu eiriolaeth yn rhad ac am ddim i bobl sy'n gymwys ar gyfer y gwasanaeth. O dan Ddeddf Gofal 2014, mae gan awdurdodau lleol ddyletswydd gofal i gynnig eiriolwr yn ystod camau asesu, cynllunio, adolygu gofal neu adolygu diogelu gofal person ar yr amod eu bod:
Mae anhawster sylweddol yn cael ei ystyried yn anhawster:
Ni all oedolyn priodol:
Hyfforddiant ar gyfer eiriolwyr
Dylai eiriolwyr annibynnol lynu at y canllawiau statudol yn neddf Rheoleiddio ac Arolygu Gofal Cymdeithasol (Cymru) 2016 (https://bit.ly/33ZpW49) a gweithio tuag at y Cymhwyster Cenedlaethol mewn Eiriolaeth o fewn blwyddyn i gael eu penodi. Cymhwyster seiliedig ar gymhwysedd yw hwn y mae'n rhaid cyflwyno tystiolaeth o arfer gweithio go iawn ar ei gyfer. Oherwydd y cysylltiad agos â'r Ddeddf Galluedd Meddyliol, gall eiriolwyr hefyd astudio unedau hyfforddi ynghylch "darparu eiriolaeth galluedd meddyliol annibynnol" a "diogelu rhag colli rhyddid".